With St. Patrick’s Day coming up I thought I’d repost this Irish blessing. Hope everyone is doing well. Happy Friday. Wishing you as pain free a weekend as possible!

Originally posted 9/22/12
With St. Patrick’s Day coming up I thought I’d repost this Irish blessing. Hope everyone is doing well. Happy Friday. Wishing you as pain free a weekend as possible!

Originally posted 9/22/12
Many of you may know that actor Morgan Freeman suffers from fibromyalgia, although from his words his pain seems to be more localized to the left side of his body injured in a bad car accident and hasn’t gone full body yet. That doesn’t mean his symptoms don’t cause havoc full body. It’s just my guess. Anyway, I stumbled upon this article where Freeman discusses his fibromyalgia pain and says that marijuana is the only thing that provides him with pain relief. He says it’s benefits are enough that it should be legalized nationwide. It’s an interesting article and a quick read so I thought I’d share it.
This survey of chronic pain sufferers is interesting. My only surprise is that some of the statistics aren’t closer to 100% of pain sufferers! I’m bolding a few things I found most interesting, including the link if you would like to participate in the survey.
Chronic Pain Sufferers Skeptical of Their Government
Readers of the National Pain Report are skeptical about their government and its role in pain management.
In April, we asked them some basic questions about the state of pain management today, and since almost all (99%) who answered online described themselves as chronic pain patients, their frustration was palpable.
When asked if the pain patient is being adequately considered in the discussion of how to address the chronic pain issue in the United States, more than four out of five (81%) said they either moderately or strongly disagreed.
When we asked about government’s role, the skepticism we mentioned was in full flower:
84% said that federal regulatory agencies like the Food and Drug Administration and the Drug Enforcement Administration are part of the problem in chronic pain treatment, and 72% said the same about elected officials.
Reader Nancy Ribok lamented the lack of education in pain management when she wrote, “doctors need to be educated on pain management, and doctors need to educate patient about pain medication and how and when to use.”
Readers who participated were less critical about their own physicians. They were equally split on whether their doctor was part of the solution (33%), part of the problem (26%) or both (27%)
We asked about the National Pain Strategy which represents “the United States first strategic plan for transforming and advancing pain care, education, research and prevention,” according to Dr. Sean Mackey, Chief of the Division of Pain Medicine at Stanford University’s School of Medicine.
The question was: “Is the National Pain Strategy asking the right questions about how to address the pain issues in the U.S.?”
Half agreed and half didn’t.
“I understand the guarded skepticism that the person living with chronic pain has about the state of pain management today and of the National Pain Strategy,” said Dan Bennett, M.D. who is Chairman of The National Pain Foundation. “However, if we are going to have the needed global conversation about acute and chronic pain, the participation of the person living with pain and those who are concerned for them is crucial. Pain is personal. The conversation must start; it is long overdue. The National Pain Strategy should be thought of in that context. We urge people living with pain, those who care about them, and advocate groups in all areas to actively participate in the public comment process.”
The National Pain Report conducts occasional readers’ surveys to gauge reaction (and also to help decide what topics to cover).
Reader Beth McDonald had a message for us and other media members when she wrote on coverage of the pain medication issues:
“To the media I would try to report on a chronic pain sufferer to enlighten the public on how pain sufferers try every possible means of pain relief before needing pain medication and why it is so vital to many in order to function.”
The people who answered the survey were mostly women who listed back pain (78%), Fibromyalgia (46%), Neuropathy and Osteoarthritis (both 44%) and Migraines (37%) as the leading causes of their pain.
We will leave the survey open for a while longer, in case you want to participate (click here)
Given my very limited knowledge of science and how the body works, I’ve been wondering for awhile if the mitochondria could be a part of what causes (or maybe fuels?) fibromyalgia. It looks like I’m not the only one wondering that and some researchers are starting to research this very thing. This article details several small studies done recently into whether FM is a mitochondrial disorder. I found this particularly interesting.
“Significant reductions in mitochondrial enzyme activity (in complexes I, II, III and IV) were found in the FM patients but not the healthy controls. That, in combination with reduced levels of mitochondrial proteins, indicated that mitochondrial functioning was indeed significantly reduced. So were CoQ10 and ATP levels and mitochondrial DNA levels. In fact, every aspect of mitochondrial functioning tested was found to have taken a significant hit in the FM patients.
“That suggested mitochondrial damage had occurred and that finding set the stage for the next test. Since damaged mitochondrial DNA are known to spark an inflammatory response, the researchers asserted they should also be able to find evidence of inflammation in the skin – and they did. Double the levels of the pro-inflammatory cytokine TNF-a were found in the skin of the FM patients.
“Not only were the increased cytokine levels strongly associated with reduced mtDNA – suggesting that the mitochondrial problems had indeed sparked the inflammation – but they were highly correlated with the pain levels in FM (p<.001) as well. That suggested the mitochondrial problems could be causing or contributing to the pain the FM patients were experiencing.
“A threefold increase in TNF-a levels in the saliva and the blood collected from the biopsy area relative to the healthy controls suggested that widespread or systemic inflammation and oxidative stress was present as well. The FM patients looked pretty much like a soup of mitochondrial dysfunction, oxidative stress and inflammation.”
And this bit makes me want to try adding CoQ10 back into my daily supplement routine. I did it years ago and didn’t notice much of a change, but maybe it’s worth trying again.
“CoQ10 is a particularly intriguing nutrient given its ability to both boost ATP production and reduce levels of oxidative stress. C0Q10 levels are reportedly low in many neurodegenerative disorders including Parkinson’s disease, diabetes, fibromyalgia and cancer.
“A fibromyalgia study by this Spanish research group found a 50% reduction in COQ10 levels in FM. With dozens of mostly small studies examining mitochondrial dysfunction and CoQ10 levels/supplementation in FM and other disorders under it’s belt, this Spanish research group has been leading the way in this area.”
I’m always on the lookout for new oils, creams, and ointments to use to give me relief from some of my fibromyalgia symptoms. One I had been using (Traumeel) just rebranded itself and changed its formula and I don’t like it as much now. Plus, it’s not available anymore on the website I order stuff like that through to make those types of products cheaper. Now I will be trying Two Old Goats products thanks to Seeking Equilibrium. It’s so stupid that they can’t brand their merchandise as treating fibromyalgia and arthritis anymore! Yet another reason for me to be mad at the FDA and get up on my soapbox. I love essential oils and lavender and eucalyptus are my go tos for aromatherapy. Lavender especially seems to work really well for me. I’m excited that these products have other natural anti-inflammatories in them like peppermint too. I can’t wait to try these out!
Read more … Two Old Goats Essential Oil Review via Seeking Equilibrium.
We all have bad days where keeping a positive outlook is impossible. Where we feel like we’ve been hit by a tractor trailer or run over by a train. We react to the weather and can predict it better than weatherpeople can. I like this blog post by Seeking Equilibrium about the average daily pain we all become accustomed to living with and the off-the-charts, please-make-it-stop pain that makes us crawl in bed and pray for sleep until the flare is over.
You know that feeling when you come home after a long, long day and fall into your oh so comfy bed and your whole body breathes a sigh of relief? Yeah, I miss that feeling. I get no such relief thanks to fibromyalgia. I wish I could experience that blissful feeling again when your whole body relaxes and melts into the bed and all the tension of the day just evaporates. I wish I could lay in my bed without experiencing pain. And not just the normal 24/7 pain of fibromyalgia, but pain caused by laying in bed. If I lay in bed too long, I get up bruised and beaten. I can’t win. Standing up and moving around hurts. Laying in bed hurts. What do you want from me, fibro monster?
I’ve had a long couple of days at work and I was exhausted when I got home today. I told myself I’ll just lay down for a bit and then I’ll get up, exercise and have some dinner. All I wanted was for my body to be able to relax and some of the tension from the last few days to leave my body. I just wanted to recharge my batteries a bit before tackling the daily (or almost every day) workout and yoga session I have to do to manage my fibro pain. I lay here willing my body to relax but the longer I lay, the worse the pain got. My legs and hips tightened up and my lower back went from tight to cramped to throbbing. My headache went from bad to worse. No matter what position I tried or how many times I got up to stretch out an aching part of my body, I couldn’t find a comfortable position that would allow my body to relax. So I finally gave up and got out of bed and started moving around. Moving around at least loosened up my painfully tight muscles a tiny bit.
Fibromyalgia changes everything in your life. It turns your life upside down. It takes away a lot of things and it makes you appreciate the little things. I used to take for granted that feeling of collapsing into bed and your whole body breathing a sigh of relief. Now, I wish I could experience it just one more time.
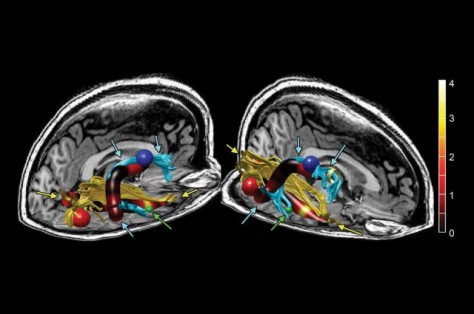
The red, blue, and green spheres correspond to size and locations of increased cortical thickness in the right occipital, precentral, and middle temporal regions, respectively. The green arrows also point to the middle temporal region of increased thickness. Credit: Radiological Society of North America
A new study by Michael Zeineh of the Stanford University School of Medicine now proves that chronic fatigue syndrome (CFS) is not hypochondria or our imagination, it is a real disease. Zeineh and his team discovered brain abnormalities in CFS patients that will hopefully help doctors to better treat this debilitating disease. There is a lot of cross over between CFS and fibromyalgia, as anyone who suffers from one or both of these devastating diseases will tell you. Patients with one of these diseases (or both) battle chronic disease, chronic pain, micro-inflammation, environmental sensitivities (such as light, smells, foods, weather, etc.) and much more every single day. So the next time you think that just because you can’t see our illness it isn’t real, think again. Thanks to researchers like Zeineh we are slowly but surely getting proof that our diseases are real and terrible.
The entire article about Zeineh’s research continues below.
Study finds brain abnormalities in chronic fatigue patients
An imaging study by Stanford University School of Medicine investigators has found distinct differences between the brains of patients with chronic fatigue syndrome and those of healthy people. he findings could lead to more definitive diagnoses of the syndrome and may also point to an underlying mechanism in the disease process.
It’s not uncommon for CFS patients to face several mischaracterizations of their condition, or even suspicions of hypochondria, before receiving a diagnosis of CFS. The abnormalities identified in the study, to be published Oct. 29 in Radiology, may help to resolve those ambiguities, said lead author Michael Zeineh, MD, PhD, assistant professor of radiology.
“Using a trio of sophisticated imaging methodologies, we found that CFS patients’ brains diverge from those of healthy subjects in at least three distinct ways,” Zeineh said.
CFS affects between 1 million and 4 million individuals in the United States and millions more worldwide. Coming up with a more precise number of cases is tough because it’s difficult to actually diagnose the disease. While all CFS patients share a common symptom—crushing, unremitting fatigue that persists for six months or longer—the additional symptoms can vary from one patient to the next, and they often overlap with those of other conditions.
Scientific Challenge
“CFS is one of the greatest scientific and medical challenges of our time,” said the study’s senior author, Jose Montoya, MD, professor of infectious diseases and geographic medicine. “Its symptoms often include not only overwhelming fatigue but also joint and muscle pain, incapacitating headaches, food intolerance, sore throat, enlargement of the lymph nodes, gastrointestinal problems, abnormal blood-pressure and heart-rate events, and hypersensitivity to light, noise or other sensations.”
The combination of symptoms can devastate a patient’s life for 10, 20 or even 30 years, said Montoya, who has been following 200 CFS patients for several years in an effort to identify the syndrome’s underlying mechanisms. He hopes to accelerate the development of more-effective treatments than now exist. (A new Stanford Medicine magazine story describes the study in more detail.)
“In addition to potentially providing the CFS-specific diagnostic biomarker we’ve been desperately seeking for decades, these findings hold the promise of identifying the area or areas of the brain where the disease has hijacked the central nervous system,” Montoya said.
“If you don’t understand the disease, you’re throwing darts blindfolded,” said Zeineh. “We asked ourselves whether brain imaging could turn up something concrete that differs between CFS patients’ and healthy people’s brains. And, interestingly, it did.”
The Stanford investigators compared brain images of 15 CFS patients chosen from the group Montoya has been following to those of 14 age- and sex-matched healthy volunteers with no history of fatigue or other conditions causing symptoms similar to those of CFS.
Three Key Findings
The analysis yielded three noteworthy results, the researchers said. First, an MRI showed that overall white-matter content of CFS patients’ brains, compared with that of healthy subjects’ brains, was reduced. The term “white matter” largely denotes the long, cablelike nerve tracts carrying signals among broadly dispersed concentrations of “gray matter.” The latter areas specialize in processing information, and the former in conveying the information from one part of the brain to another.
That finding wasn’t entirely unexpected, Zeineh said. CFS is thought to involve chronic inflammation, quite possibly as a protracted immunological response to an as-yet unspecified viral infection. Inflammation, meanwhile, is known to take a particular toll on white matter.
But a second finding was entirely unexpected. Using an advanced imaging technique—diffusion-tensor imaging, which is especially suited to assessing the integrity of white matter—Zeineh and his colleagues identified a consistent abnormality in a particular part of a nerve tract in the right hemisphere of CFS patients’ brains. This tract, which connects two parts of the brain called the frontal lobe and temporal lobe, is called the right arcuate fasciculus, and in CFS patients it assumed an abnormal appearance.
Furthermore, there was a fairly strong correlation between the degree of abnormality in a CFS patient’s right arcuate fasciculus and the severity of the patient’s condition, as assessed by performance on a standard psychometric test used to evaluate fatigue.
Right vs. Left
Although the right arcuate fasciculus’s function is still somewhat mysterious, its counterpart in the brain’s left hemisphere has been extensively explored. The left arcuate fasciculus connects two critical language areas of the left side of the brain termed Wernicke’s and Broca’s areas, which are gray-matter structures several centimeters apart. These two structures are important to understanding and generating speech, respectively. Right-handed people almost always have language organized in this fashion exclusively in the left side of the brain, but the precise side (left or right) and location of speech production and comprehension are not so clear-cut in left-handed people. (It’s sometimes said that every left-hander’s brain is a natural experiment.) So, pooling left- and right-handed people’s brain images can be misleading. And, sure enough, the finding of an abnormality in the right arcuate fasciculus, pronounced among right-handers, was murky until the two left-handed patients and four left-handed control subjects’ images were exempted from the analysis.
Bolstering these observations was the third finding: a thickening of the gray matter at the two areas of the brain connected by the right arcuate fasciculus in CFS patients, compared with controls. Its correspondence with the observed abnormality in the white matter joining them makes it unlikely that the two were chance findings, Zeineh said.
Although these results were quite robust, he said, they will need to be confirmed. “This study was a start,” he said. “It shows us where to look.” The Stanford scientists are in the planning stages of a substantially larger study.
More information: “Right Arcuate Fasciculus Abnormality in Chronic Fatigue Syndrome” Radiology, 2014.
Thanks to Seeking Equilibrium, I discovered FibroGuide. FibroGuide has a modules with great information for those newly diagnosed and those of us who have had fibromyalgia for what feels like forever. You take a simple quiz and it points you to the modules you may find most helpful. Examples of modules are Understanding Fibromyalgia, Fibro Fog, Being Active, Communicating, Sleep, Pacing Yourself, and more. It’s got a lot of great information and I really like how it’s organized. With the quiz, you are quickly pointed to the resources you may find most helpful and don’t have to go digging through a ton of information for the tidbits that are the most relevant for you. I don’t know about you, but my attention span is short and my thoughts are easily scattered so I found the way this site is organized to be very helpful. Check it out!
Reblogged from Seeking Equilibrium
I’ve gone through a “roadkill tired” spell myself of late. I think I’m finally coming out of it. Adding a Vitamin B and iron supplements to my daily mix of supplements seems to be helping me feel a more normal level of tired, not the bad roadkill tired I’ve been doing. My brother actually figured out that it sounded like I was iron deficient. I definitely notice a difference now that I’m taking it. Thanks brother!
This post on chronic fatigue as it relates to fibromyalgia and other chronic illnesses is really great. She highlights ten common suggestions doctors make to help decrease fatigue and how most of them really work for fibro sufferers. Our brains just don’t work like “normal” brains and until doctors realize that and modify their recommendations accordingly, we’re stuck with getting the same unhelpful advice over and over. My favorite tip she makes is:
Point number 10: Be good to yourself. There is a lot of guilt and problems that go with chronic illness. We do need to be good to ourselves. This will be with us until there is a cure so we shouldn’t be too hard on ourselves.
I love these graphics. Sometimes the best way to understand a bunch of statistics and data is visually. I know I’m a visual learner. The only thing I don’t like about these graphics is that the statistic on how many women have fibromyalgia should be how many people. Men get fibromyalgia too. This is not just a “woman’s disease.”
Image and statistics courtesy of MBA Healthcare Management and Seeking Equilibrium.
I’ve been working through a lot the past year and a half, and perhaps most especially the last few months. I came across this this morning and it struck a chord so I wanted to share. I think of all the lessons I have learned, “You will relapse and that’s okay – as long as you keep fighting,” is the most important. I’ve been frustrated by the feeling that I recover from one physical ailment just to have another one come at me that I have to deal with. Life is a rollercoaster sometimes and sometimes all you can do is roll with the ups and downs as they come. I’ve also learned to get the most enjoyment out of the “ups” as I can. It’s important to enjoy those times while they last. They help you get through the “downs.”
“In the confrontation between the stream and the rock, the stream always wins not through strength, but through persistence.” –Peter Davies