Many of you may know that actor Morgan Freeman suffers from fibromyalgia, although from his words his pain seems to be more localized to the left side of his body injured in a bad car accident and hasn’t gone full body yet. That doesn’t mean his symptoms don’t cause havoc full body. It’s just my guess. Anyway, I stumbled upon this article where Freeman discusses his fibromyalgia pain and says that marijuana is the only thing that provides him with pain relief. He says it’s benefits are enough that it should be legalized nationwide. It’s an interesting article and a quick read so I thought I’d share it.
Tag Archives: symptoms
The Weather and the Very Icky Day
We all have bad days where keeping a positive outlook is impossible. Where we feel like we’ve been hit by a tractor trailer or run over by a train. We react to the weather and can predict it better than weatherpeople can. I like this blog post by Seeking Equilibrium about the average daily pain we all become accustomed to living with and the off-the-charts, please-make-it-stop pain that makes us crawl in bed and pray for sleep until the flare is over.
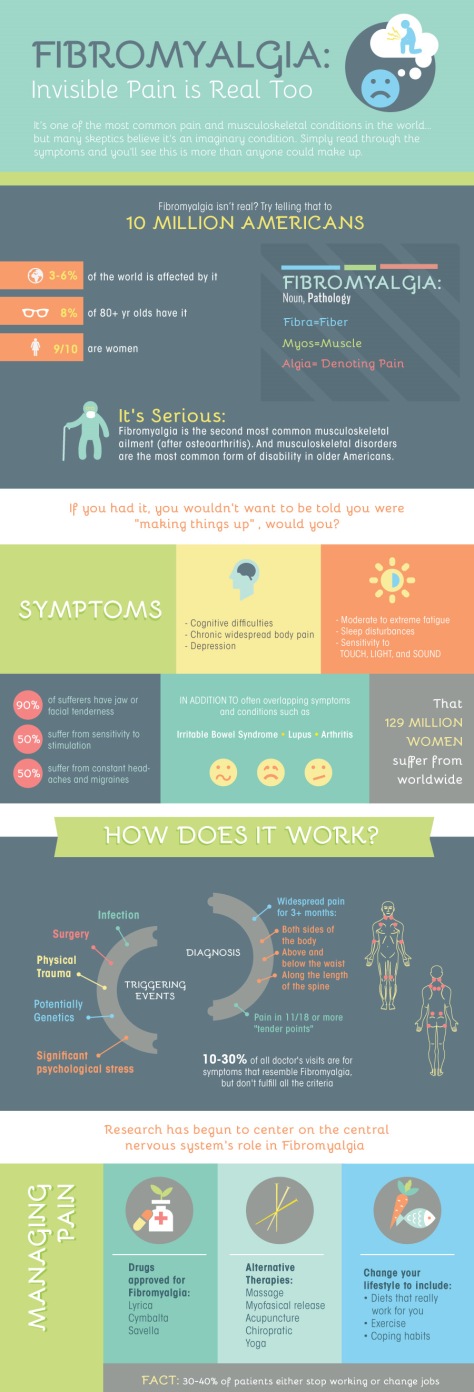
Fibromyaglia is Real
I love these graphics. Sometimes the best way to understand a bunch of statistics and data is visually. I know I’m a visual learner. The only thing I don’t like about these graphics is that the statistic on how many women have fibromyalgia should be how many people. Men get fibromyalgia too. This is not just a “woman’s disease.”
Image and statistics courtesy of MBA Healthcare Management and Seeking Equilibrium.
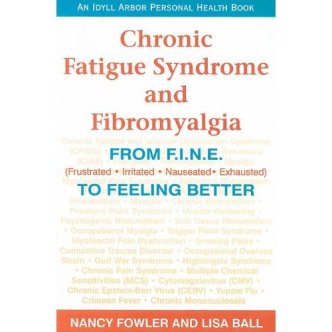
From Fine to Feeling Better, a Fibromyalgia Book Review
I recently read Chronic Fatigue Syndrome and Fibromyalgia: From F.I.N.E. (Frustrated, Irritated, Nauseated, Exhausted) to Feeling Better. This is a good book for the newly diagnosed and a good refresher for those who have had Chronic Fatigue Syndrome and/or Fibromyalgia for a while. This book is very upbeat. It makes both diseases seem less daunting. It is similar to a short textbook in that it covers a wide range of topics relating to both diseases as well as focusing on how to help you feel better. The authors of this book — Nancy Fowler and Lisa Ball — describe both diseases, but especially fibromyalgia I think, as “The Thief.” Fibromyalgia steals much from us and changes much in our lives. I think their name for this invisible disease is very apt.
The book aims to educate the reader about his/her disease and to help he/she to cope with the all of the symptoms and changes these diseases force on us. The authors discuss a wide range of topics — from how CFS and fibromyalgia manifest physically to how they affect people mentally and emotionally. This is a good, positive book. I think the way it is most helpful is that each chapter is on a different topic relating to both diseases. You can look at the table of contents and identify the chapters that are most relevant to you and just read those. This is a good thing for us as “fibro fog” often keeps us from being able to focus for more than a short period of time on something detailed like a book. Fibromyalgia and all the medications we have to take to cope with it impair our ability to focus. I believe the authors understood this and set their book up to very reader friendly.
I read much of this book but two chapters resonated the most with me: Nutrition and Psychological Aspects of these diseases. This book is the first place I have seen a detailed list of nutritional concerns and suggestions specifically for sufferers of fibromyalgia and/or CFS. The nutrition chapter was my favorite by far and it had really good suggestions in it that are easy to apply in your daily life. They are simple suggestions to help you feel better, not daunting life changes that require lots of energy and effort.
Here are some of the book’s suggestions from the nutrition and psychological chapters that I jotted down to keep in mind for myself.
Nutrition:
- Proteins (meat, poultry, fish, tofu and cottage cheese) will ease carb cravings, give you added energy and aid in weight loss.
- Omega-3 fatty acids have anti-inflammatory properties. Fish oil supplements are a good idea for sufferers of fibromyalgia and CFS.
- Drinking lots of water MUST. Water hydrates cells and flushes toxins out of the body.
- Don’t drink carbonated beverages. Sugar brings an initial energy spike that soon fades, causing a roller coaster effect. Each carbonated drink as 12-14 tsp. of sugar and can lead to yeast problems.
- Small amounts of dark chocolate are good for you. Most chocolate candy is high in fat and has a small amount of caffeine. Stay away from these and caffeine in general.
- Stay away from MSG. It can cause headaches, dizziness, and chest pain.
- Beauty products can contain allergens (gluten, for example). (I recommend Neutrogena makeup products as they are gluten free and very safe.)
- Look for and avoid Aspartame. It’s usually in diet/sugar-free foods.
- Steaming preserves more of the “good stuff” in foods than boiling.
- Don’t eat too many carbs.
Psychological Aspects:
- The 5 stages of grief apply to fibromyalgia: Denial, Anger, Bargaining, Depression, Acceptance.
- We move through these stages but eventually we have to accept that these diseases are part of our lives and move on with our life. Anger, depression, and self-pity all help pain to flourish. There is a huge emotional component to fibromyalgia. These types of feelings help feed our pain.
- Once you accept this, then you can start to control your life and body again. Then the healing process can truly begin. You won’t be on a constant emotional roller coaster anymore. You can find yourself again and be you again.
I recommend reading Chronic Fatigue Syndrome and Fibromyalgia: From F.I.N.E. (Frustrated, Irritated, Nauseated, Exhausted) to Feeling Better. When reading it, keep in mind that the authors are big believers in the power of positive thinking and the power of faith. Your views on these topics may not be the same as theirs, but the authors still provide really good information in this book. If they get too much into the positive thinking and faith side of things, just skip that part and move onto the next section. Despite this minor flaw, this book is still a very helpful resource for those suffering from fibromyalgia and/or CFS.
Quote of the Day
“Victory is always possible for the person who refuses to stop fighting.”
–Napoleon Hill
Maybe if we just keep fighting, and work every day to get a little bit better, one day our fibromyalgia/chornic pain will just go away. Or someone will develop a drug that reduces our symptoms. What a victory that would be!
Fibro Symptom Tracker
Check this out. There’s an app called “Manage My Pain” that can help us track our symptoms. You can even run reports on the app and send it to people. Maybe it will help us track the good days and bad days and our triggers.
Read the agreement/conditions text carefully though. I got the Lite version since it’s free, but it talks about the app creator using our data as “aggregate data” to track how the app is working. I assume that is more like which features to we use and how often are they used. It also says if you send the reports to people, they may capture your info as well as any names/emails of who you send it to. I don’t know what they’d do with it, but read it carefully and decide if that’s okay by you. I agreed because I wanted to play with the app and see if it’s helpful to me. I’ve been thinking of late that I need to keep a symptom journal, but I’m always bad about remembering to do daily entries. I think I am more likely to keep up with it daily in an electronic format I can use on my phone and hopefully on my Kindle Fire too. I don’t think I’ll be sending anyone reports since they may capture that data though. I just wanted to warn everyone of that buried fine print.
I’m going to play with this app and will update you on what I think of it.
Here’s more detailed info on the app: http://www.scenarhealthcanada.com/manage-my-pain/.
Thankful Thursdays – Week 2 – Change
I’m doing my Thankful Thursdays writing challenge a bit different today. I wanted to share this poem with you that Fibrozine was nice enough to post.
Chronic Pain and Changing your Life Plan
This is so very true. I’m struggling a lot with this too. It’s something my husband and I are working on together. The plan we had for our lives did not include me developing fibromyalgia and all the ramifications that brings. Things have to change and we don’t exactly know what that means for the future. We’re working on it. I’ve had to make a lot of changes to myself, my thoughts, and my habits. I’ve had to drop down to only working 30 hours a week at my job instead of working a full 40 hours. Lots of things are changing right now and it takes some getting used to for me, my husband, my family and my friends. I’m not the same person I was before fibromyalgia. Chronic pain has changed me. I think some of the ways I’ve had to change are for the better. I appreciate the little things now more than I ever did before. Other changes have been by necessity and take some getting used to.
I’ll figure out my new life plan. My husband and I will figure out our new future together, I hope. I’ll get there. It’s a long but necessary journey.
Useful Info from Pain Awareness Month
I’ve really been getting in to promoting September as Chronic Pain Awareness month and National Chronic Invisible Illness week this week. It’s comforting to me that there are those out there working hard to raise awareness for what we chronic pain sufferers go through every day. It’s great to know that there is support for us out there and people rooting for us, even though we’ve never met them.
I was looking at American Chronic Pain Association’s website and found this link. It has some useful information and tools for chronic pain sufferers that I wanted to share. Topics include lessons learned on treating chronic pain medically, information on pain management programs, a relaxation video (which I haven’t looked at yet because I’m at work), tools to help us communicate our symptoms and needs better to our doctors, and lots of other resources.
I used this site’s rescoure finder and the first thing that popped up for me was an interesting article on the history of diagnosing and treating fibromyalgia. I didn’t realize that the diagnosis of an earlier understanding of fibromyalgia dates back to 1800.
http://www.theacpa.org/69/Septemberispainawarenessmonth.aspx
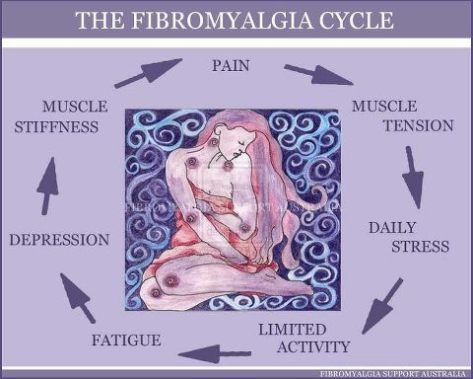
The Fibromyalgia Cycle
This is one of the best graphic representations of the fibromyalgia cycle I’ve ever seen, so I had to share. Based on my own personal fibromyalgia symptoms, I would make a few changes though, if this were my drawing. I would change fatigue to Fatigue/Poor Sleep. Sleep is key for fibromyalgia sufferers. I need a minimum of 8 hours a night. I don’t always get that, but I do my best to come close. Even if I do get 8 hours, its usually not a full 8 hours of good, restful sleep. Our bodies need a chance to recharge and get a break from the havoc our brain’s screwed up pain signal wiring causes. Sleep gives us this necessary break. Without sleep, we are fatigued and our pain is worse.
I’d also change limited activity to Limited or Too Much activity. Too little exercise or activity can increase our pain, but so can overdoing it. If we have a good day and push ourselves too hard, we’re going to pay for it the next day with more pain.
I’d also change Depression because it isn’t just that emotional state that feeds our pain. Any extreme emotion will do it. I’ve had a long crying fit trigger a fibro flare up, but I’ve also had a really good day where I was super excited and almost manically happy trigger a flare up. If we go too far to either side of the scale, we’re going to pay for it with more pain the next day.
All of these triggers feed our pain. They all feed eachother. They all form a vicious cycle that just causes all these symptoms to get worse and worse. It’s incredibly hard to break this cycle. Medications can help. A daily exercise program can help. Working with a cognitive therapist can help. But most of all it takes willpower and inner strength to pick a symptom, target it mentally, and work to make it better. If I can make one of these symptoms better, my pain gets a little better. If I can balance these symptoms so they’re all in a more normal range, my pain drops to the lowest level, which I call my good days. It’s like keeping plates balanced and spinning on poles. It’s hard and nearly impossible, but it’s really cool when you achieve it.
Doctors can be part of the problem
I was my typical clutzy self this morning and managed to cut my thumb while trying to slice up a watermelon. It looked worse than it actually is, so I went to my local urgent care clinic. My thumb is fine and I didn’t need stitches, but just going to urgent care stressed me out. It was the same urgent care place I went to when my pain first started in college. It was the same long wait, the same rude staff, the same clueless doctor. Back then, my chronic pain began with stabbing pains in my leg. Leg pain became hip and back pain, which became shoulder and neck pain, which became a bad migraine, and the next thing I knew, every part of my body hurt. It took me 3 years and countless doctors to figure out that my TMJ disorder was the cause of my pain returning and spreading throughout my body. It took another year and half to get the fibromyalgia diagnosis.
Doctors can be part of the problem when you are facing a chronic health problem.
That first doctor at urgent care examined me for about 10 minutes, prescribed Darvocet, and told me to deal with the pain. He was oh so helpful. I didn’t take the Darvocet more than once. I couldn’t function on it. It was too strong a prescription for the level of pain I had then. I moved from one doctor to the next, always searching for what was wrong with me. Not knowing what is wrong with you is the absolute worst. You imagine all the things that could be wrong and you scare yourself silly. Then doctors start talking about all these even more horrible diseases than you thought of, and then you’re scared out of your mind. I had X-rays done of my legs, back, neck, and jaw. I had two MRIs done. I lost count of all the different bloodwork that was ordered. I did exclusion diets to see if somehow this was allergy related. I repeatedly changed the exercises I was doing just in case something I was doing was making things worse. I saw a sports therapist to learn how I should be stretching. I saw a chiropractor who helped me some but kept leading me on to pad his bank account. I tried acupuncture and massage therapy. I saw osteopaths and MDs. I did physical therapy for 6 months. They tried a coritzone shot to my jaw (which really hurts by the way). They checked my eyes in case they were part of the problem. I even convinced my eye doctor to give me a just less than optimal prescription for glasses and contacts because I had read that an optimal prescription can actually make chronic pain worse. You name it and I’ve probably tried it.
You have to educate yourself about your symptoms so you know the right questions to ask your doctor. If you don’t like his/her answers, try a different doctor. Find a specicalist. If he/she doesn’t help you, try a different specialist. Keep going from one doctor to another until you find one that you trust 100%. Once you find that doctor, he/she can suggest other good doctors to you. You just have to weed out all the unhelpful doctors before then. It’s not that these doctors are bad, necessarily, its that they were trained a certain way and they can’t think outside the box. When you’re dealing with something systemic like fibromyalgia that involves neurological, physical and emotional pain and trauma, you need someone who will think outside of the box. You need a doctor who is willing to say “I don’t know the best way to treat you but I’m going to find out.” Doctors like that are rare in my experience.
It’s taken me almost 9 years now, but I’ve assembled a core group of doctors and therapists who I trust completely. They work to help me get better. They don’t just throw a prescription at me and send me on my way. If something doesn’t work, they figure out a new treatment alternative to try. I see my family doctor, osteopath, EMDR therapist, cranial massage therapist, orthodontist, and acupuncturist regularly. Most of them keep in touch with each other to monitor my treatment. If they don’t talk to each other, I update them on what the others are doing so they all have a complete picture of my treatment plan.
Doctors can be part of the solution…but they have to be the right doctors for you. Everyone has different needs. It makes sense that we’d need different doctors to help us through our chronic health problems. If you don’t have a doctor you like and trust, it’s time to start looking for one. Seeing the wrong doctor is a waste of your time, energy and money. It’s frustrating and tiring to keep looking for the right doctor, but trust me, it’s worth it.
Chronic Pain and Your Mental Health
Reblogged from Allied Spine and Neurology:
Results from a new study by Gallup-Healthways show that 47% of American adults suffer from chronic pain. The American Chronic Pain Association defines chronic pain as “pain that is ongoing or recurrent, lasting beyond the usual course of acute illness or injury or more than 3 to 6 months, and which adversely affects the individual’s well-being.”
According to the Harvard Mental Health Letter, people with chronic pain have three times the average risk of developing psychiatric symptoms – usually mood or anxiety disorders. It is certainly easy to understand how a person with chronic pain can develop symptoms of depression and/or anxiety. There is a physical and an emotional toll as chronic pain often limits what a person can do. Many people say that their pain symptoms fluctuate and can be tolerable one day but incapacitating the next day. Not knowing what to expect from day to day can produce anxiety and interfere with meaningful relationships. It can also result in isolation as people refrain from making plans for fear of a flare-up with their pain. Chronic pain results in varying degrees of immobility and curbs one’s activities of daily living. The inability to function can result in both anxiety and depression, and when coupled with self-imposed isolation, chronic pain sufferers are at considerable risk for severe depression. If depression becomes part of the equation, chronic pain can significantly worsen as patients endure increased fatigue, insomnia, and a weakened immune system, all of which impact pain. Depression also interferes with pain signals and can result in extended pain.
Patients with chronic pain need to have a multi-disciplinary approach to treatment, one that includes some element of support. People living with chronic pain understand that there will be “good” days and “not so good” days, but the key is to continue using the positive words. Employing effective coping mechanisms will also give chronic pain patients a feeling of control during a time when they might feel that they have no control over their situation. Patients are encouraged to talk about their conditions and to focus on their abilities rather than their disabilities. By setting short-term achievable goals, patients can see and feel their progress. Learning relaxation techniques will lessen tension in the body, thereby lessening pain caused by muscle tightness and/or spasms.
The American Chronic Pain Association has created a list of basic rights for chronic pain sufferers.
Here are a few examples. You have the right to:
- Be treated with respect.
- Feel good about yourself.
- Take time to slow down and think before you act.
- Ask for information.
As part of the information gathering process, if you or a loved one is suffering from chronic neck pain or chronic back pain, please contact Allied Neurology and Interventional Pain Practice today. We have many treatment options available to address your chronic pain including interventional pain management and minimally invasive surgical procedures. Our treatment goals include a reduction in pain and a restoration of function that will enable patients to enjoy their activities of daily living.